Credentialing
We are offering a simplified and efficient credentialing process for healthcare providers and practices. Our array of services covers essential steps, facilitating a seamless journey for providers to become in-network and ensuring prompt reimbursements from insurance companies.
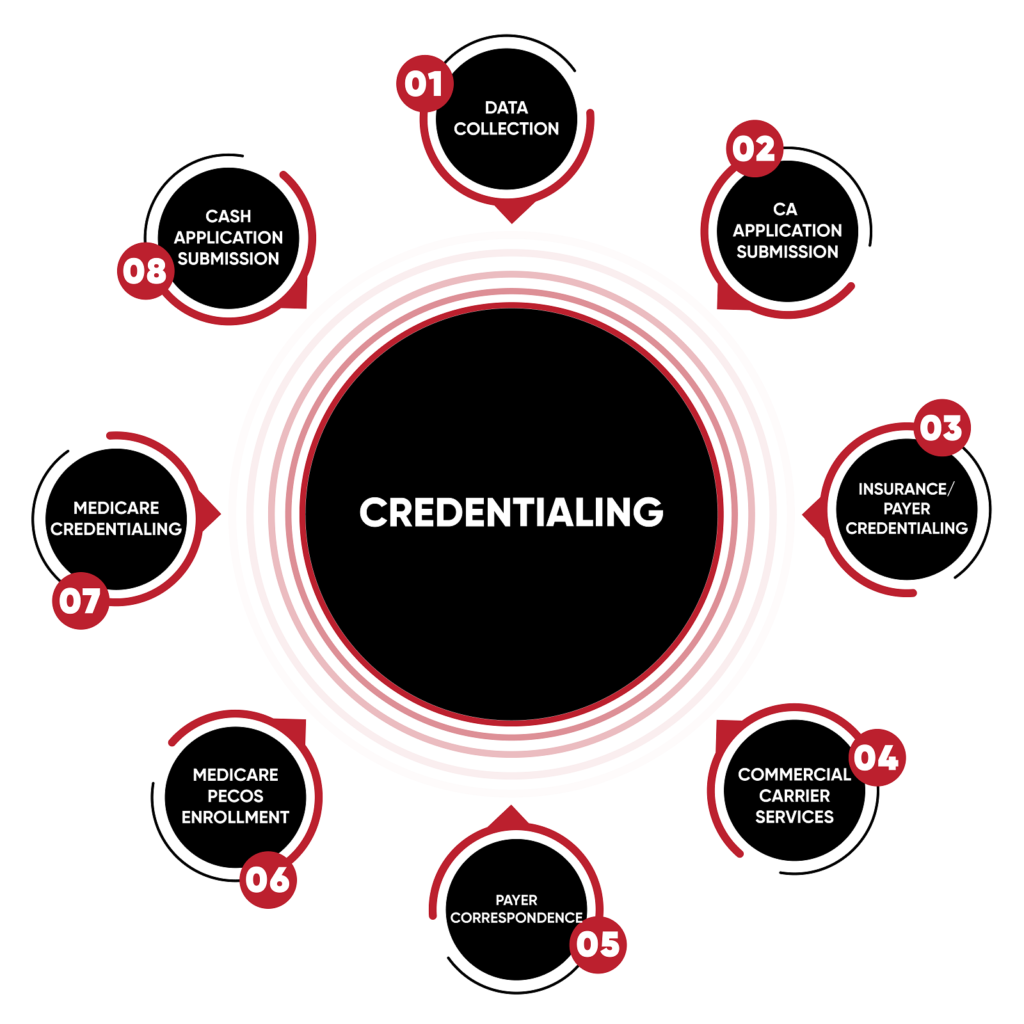
OUR STEP-BY-STEP PHYSICIAN CREDENTIALING PROCESS

Data Collection Assistance

Application Processing

Insurance/Payer Credentialing

Commercial Carrier Services

Payer Correspondence

Medicare & PECOS Enrollment

Medicaid Credentialing
CAQH Application Submission
Our dedicated team aids providers and practice administrators in gathering vital background and demographic information, establishing a solid foundation for a hassle-free credentialing process.
Once we possess all necessary documentation, we meticulously prepare and submit the requisite applications to insurance carriers, streamlining the initial stages of the credentialing process.
Tailoring our approach to payer-specific requirements, we navigate the complexities of insurance/payer credentialing, expediting reimbursement for services rendered by healthcare practices.
Extending our expertise beyond government-administered plans, we provide services for health insurance plans, ensuring comprehensive coverage and efficient credentialing for Apna MBC clients.
Our team manages all aspects of payer verifications, communications, and follow-up tasks, fostering effective and transparent interactions with insurance providers.
Guiding physicians, agencies, and medical providers through the Medicare credentialing process, we play a pivotal role in the Medicare supply chain. Additionally, we assist physicians in enrolling in PECOS to guarantee the seamless delivery of necessary care and supplies to patients.
Managing the credentialing process for agencies, medical providers, and physicians as part of the Medicaid supply chain, we ensure a smooth and efficient enrollment process for Apna MBC clients.
For physicians and providers requiring CAQH (Council for Affordable Quality Healthcare) credentialing, we manage the submission process, streamlining applications for individual payer credentialing.
Credentialing at Apna MBC comes with numerous advantages:
Comprehensive Credentialing Services: Our team provides knowledgeable and comprehensive services, offering tailored recommendations based on an analysis of Apna MBC’s service area and specialty.
Ongoing Credentialing Support: Recognizing that credentialing is a continuous process, we provide services for existing practices, handling re-credentialing, maintaining CAQH profiles, and notifying Apna MBC clients of expiring documents.
Tailored Credentialing for All Practices: Whether a solo practitioner or part of a large group, Apna MBC’s experts handle Medicaid, Medicare, and Commercial Payer credentialing for both individual and group enrollments.
Benefits of Apna MBC's Credentialing Services:
- Knowledgeable Staff: Our credentialing team navigates paperwork with expertise, ensuring a seamless process for Apna MBC providers.
- Frequent Updates: Apna MBC clients receive regular updates on credentialing status, staying informed throughout the process.
- Time for Quality Care: With reduced operational costs, Apna MBC’s providers can focus on delivering quality patient care.
- Appeal Assistance: We provide support with appeals for panel closures, ensuring Apna MBC can continue serving patients without disruptions.
- Quicker Payments: Apna MBC experiences faster payments from third-party payers, optimizing the revenue cycle.
- Major Provider Enrollment: We handle Medicaid and Medicare enrollments for both individuals and groups, ensuring comprehensive coverage for Apna MBC.
